-
Individualized Medicine
Science Saturday: Researchers seeking to identify families at risk for cancer
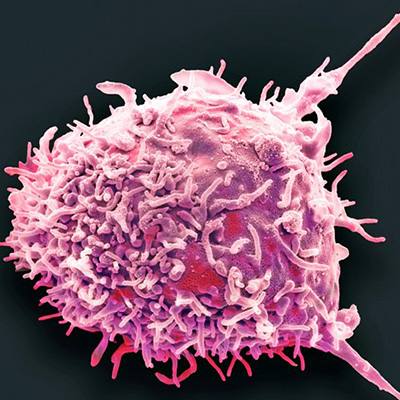
 March is colorectal cancer awareness month — a time to look at the new role of genetics in preventing and treating a common form of cancer that often runs in families. Physician-researchers within Mayo Clinic’s Hereditary Cancer Clinic are seeking to usher in a new era of identification and prevention for those with inherited risk of cancer. With support from the Center for Individualized Medicine, they are offering DNA blood testing to all patients with colon, breast, ovarian, prostate, brain and other cancers. The goal is to identify patients with genetic mutations that are putting them and their families at increased risk for cancer and respond with a proactive, individualized approach.
March is colorectal cancer awareness month — a time to look at the new role of genetics in preventing and treating a common form of cancer that often runs in families. Physician-researchers within Mayo Clinic’s Hereditary Cancer Clinic are seeking to usher in a new era of identification and prevention for those with inherited risk of cancer. With support from the Center for Individualized Medicine, they are offering DNA blood testing to all patients with colon, breast, ovarian, prostate, brain and other cancers. The goal is to identify patients with genetic mutations that are putting them and their families at increased risk for cancer and respond with a proactive, individualized approach.
Niloy “Jewel” Samadder, M.D.: “Offering hope of prevention”

As a young physician-researcher, Niloy Jewel (Jewel) Samadder, M.D., treated many patients with early onset colon and breast cancers. That inspired him to conduct research into the molecular origins of their cancer.
“If we could find a genetic cause to their cancer, then maybe we could intervene earlier to try to prevent future cancer altogether,” says Dr. Samadder. “Perhaps even more important, we could give patients hope of preventing cancer in the people they love. We could alert close family members that they may be at risk and should be screened regularly to catch cancer at its earliest stage.”
Dr. Samadder notes that 50 percent of all cancers that are precipitated by an underlying genetic mutation are missed using current guidelines – a missed opportunity for families. It is estimated that between 10 and 20 percent of cancers may have an inherited predisposition depending on the cancer type that is inherited in families. Since there are genetic conditions, your family is key: Dr. Samadder says if you have hereditary cancer, there’s a 50 percent chance your closest relatives — mother, father, sisters, brothers, sons or daughters — will have the same genetic mutation that could develop into cancer. Understanding genetic risk of cancer can focus attention on more intensive screening and monitoring. Some patients may even opt for pre-emptive surgeries to prevent cancer from occurring.
A gastroenterologist with a focus in genetics, Dr. Samadder’s cancer research centers on three main areas:
- Understanding how family history contributes to colorectal cancer risk.
- Understanding when to start chemotherapy pre-emptively to prevent cancer altogether, a concept called “chemoprevention.”
- Understanding how to integrate genetics as the regular, daily standard of care for patients with inherited cancer.
“Genetic testing not only helps us identify patients with inherited cancer, it also helps us find the root cause. This may help inform treatment decision-making, which can be targeted toward the specific genes that contribute to tumor growth. We can also consider intervening to prevent new cancer in both the patient and relatives who have the same genetic mutations,” says Dr. Samadder.
Dr. Samadder’s extensive training and experience have come full circle. Early in his career he trained at Mayo Clinic and at the University of Michigan. He then spent many years in cancer-genetics research at the University of Utah’s Huntsman Cancer Institute. Dr. Samadder returned to Mayo Clinic in mid-2017, where he sees patients on Mayo’s Arizona campuses.
“What brought me back to Mayo was its patient-first focus. Mayo stands apart in the way it brings together the three shields of education, research and practice to address the unmet needs of patients and deliver hope and healing,” says Dr. Samadder.
Douglas Riegert-Johnson, M.D.: “A new paradigm in cancer treatment”
Faster and cheaper genetic testing has led to a new paradigm in cancer prevention and treatment, according to Douglas Riegert-Johnson, M.D., who leads the Hereditary Cancer Clinic on Mayo Clinic’s Florida campus. In the past, genetic testing for hereditary cancer traits was offered selectively only to a few cancer patients.

“We’re moving to a model in which almost all cancer patients will have genetic testing for hereditary cancer traits. This information can be important for both cancer treatment and prevention. For example, if we find that a genetic mutation is the cause of a woman’s ovarian cancer, she will receive a different, more aggressive form of chemotherapy than if she didn’t,” says Dr. Riegert-Johnson.
On the prevention side, patients can take steps to prevent a second cancer. For example, a colon cancer patient with the Lynch syndrome cancer trait will have colonoscopies more frequently to prevent a second colon cancer. People with Lynch syndrome, a genetic condition, have a high risk of colon, endometrial, ovary, stomach and other cancers. The children of the patient with Lynch syndrome colon cancer can also be tested for the Lynch syndrome trait. If the test results are positive, they can begin having colonoscopies earlier and more frequently. Research shows patients who know they have hereditary cancer traits and take preventive measures do live longer, says Dr. Riegert-Johnson.
A gastroenterologist and medical geneticist, Dr. Riegert-Johnson has been practicing at Mayo Clinic since 1999 — the last 10 years in Florida. He began his training at Mayo Clinic in general internal medicine, and then studied classical genetics at Johns Hopkins Hospital. Dr. Riegert-Johnson now specializes in GI-tract hereditary cancers.
“I deal with all types of hereditary cancer. I counsel patients on what types of things they can do to prevent cancer including lifestyle changes and what tests would be useful to them or not useful to them,” says Dr. Riegert-Johnson.
During the course of his career, he’s seen cancer take a stressful toll on many families. He is drawn to the work in hereditary cancer by the potential he sees to help cancer patients live longer, higher quality of lives.
“For me, the most personally gratifying thing is to give people good news. A lot of patients have relatives with genetic mutations that predispose them to cancer. And, these patients assume they, too, have inherited cancer-causing genes. If you test them and find they are negative, you can tell that a big weight has been lifted off their shoulders,” says Dr. Riegert-Johnson.
Join the conversation
For more information on the Mayo Clinic Center for Individualized Medicine, and how it is transforming care through the discovery, translation and application of precision medicine research, visit our blog, Facebook, LinkedIn or Twitter at @MayoClinicCIM.
Save the date for this year’s Individualizing Medicine Conference. It will be held Sept. 12-13, 2018 in Rochester, Minnesota.
Related Articles