-
Individualized Medicine
Science Saturday: Mayo researchers explore genetics behind COVID-19 outcomes

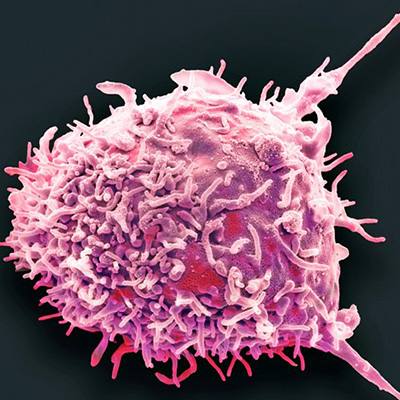
Some patients with COVID-19 experience severe complications, such as organ damage, shortness of breath, neurological impairment and chronic fatigue. A team of researchers within Mayo Clinic Center for Individualized Medicine is contributing to the global effort of using advanced genetic sequencing to find out which genes influence disease outcomes.
“Our findings will be crucial in treating and caring for COVID-19 survivors, as well as to try to prevent lingering complications in newly infected people,” says Konstantinos Lazaridis, M.D., the Everett J. and Jane M. Hauck associate director of Mayo Clinic Center for Individualized Medicine.
Dr. Lazaridis and his team are building a library of genomic sequencing data of consented patients who tested positive for COVID-19. They are using a comprehensive technology that can analyze 20,000 genes that code for proteins, plus hundreds of thousands of other genetic areas outside the protein-coding regions that are known to be informative, and thus have the most impact on a person's health and disease.
“Our aim is to answer questions about genetic predisposition of developing the infection and the long-term outcomes of the disease,” he says. “We may be in a position to say why some patients with COVID-19 develop blood clots or a severe inflammatory reaction. Or, why some patients have neurologic impairment while others show no symptoms at all.”
Why do some people possess immunity to COVID-19?

Another research team has developed an integrated model to study the genomic and non-genomic factors in the blood of people exposed to COVID-19 to understand a person’s likelihood of developing an infection, as well as the anticipated course of the disease.
“Clinical factors such as age, race, underlying conditions and certain blood markers have been reported to be associated with increased vulnerability to infection and mortality,” says Pooja Advani, M.B.B.S., M.D., who serves in the Department of Hematology and Oncology.
Dr. Advani says the fundamental question that remains unanswered is, post-exposure, who will develop the infection, and among these people, who is less likely to have a severe versus asymptomatic, or mildly symptomatic infection.
“Most investigations to date have focused on infected patients with moderate to severe clinical disease in an effort to identify high-risk or vulnerable population,” explains Dr. Advani. “Equally important is the recognition of those individuals that possess inherent biological immunity.”

The team is using their model to help predict three potential clinical pathways of a person exposed to COVID-19:
- Exposed to the virus but will not become infected
- Infected but remains asymptomatic or mildly symptomatic
- Develops aggressive disease
“The clinical spectrum of disease could further support the notion that genomic and non-genomic factors unique to a person may be responsible for the severity, or lack thereof, of the clinical impact of COVID-19,” says Dr. Advani.
Dr. Advani says identifying and understanding all the unique factors contributing to disease severity may help to modify the course of COVID-19 and improve patient outcomes.
Learn more
Read more stories about advances in individualized medicine.
Register to get weekly updates from the Mayo Clinic Center for Individualized Medicine blog.
Join the conversation
For more information on the Mayo Clinic Center for Individualized Medicine, visit Facebook, LinkedIn or Twitter at @MayoClinicCIM
Related Articles