-
Research
Science Saturday: Mayo Clinic doctor visits of the future could be powered by ‘omics’ research

To glimpse the future of medicine, step inside Mayo Clinic's cutting-edge Center for Individualized Medicine. There, physicians, researchers, data scientists, artificial intelligence engineers and bioethicists are working side-by-side to investigate massive "omics" data sets. The innovative approach is the result of thousands of patients who are participating in omics-related research studies and clinical trials.
The multidisciplinary teams are in pursuit of discovering hidden biological signatures and patterns of diseases, including cancer. Their hope and expectations are to further develop impactful individualized treatments and preventative strategies for everyone.
Meanwhile, research participants are learning if they carry certain disease-causing mutations. For now, specific genomic findings can be included in each patient's electronic health record to guide their personal health care, including potential individualized treatments and screenings. In the near future, additional omics (proteomics, pharmacogenomics, metabolomics, exposomics, etc.) could be included to create a razor-sharp individualized roadmap for their health and wellness.
"I believe this incredible amount of omics data is going to change the way we practice family medicine," says John Presutti, D.O., a Mayo Clinic family medicine physician. "We're going to most likely see significant changes as quickly as two to five years from now."
Omics is an emerging multidisciplinary field of biological sciences that encompasses genomics (study of genes), proteomics (study of proteins), exposomics (study of cumulative environmental exposures), transcriptomics (study of gene expression at the mRNA level), pharmacogenomics (study of how genes affect response to drugs), metabolomics (study of small molecules) and more.
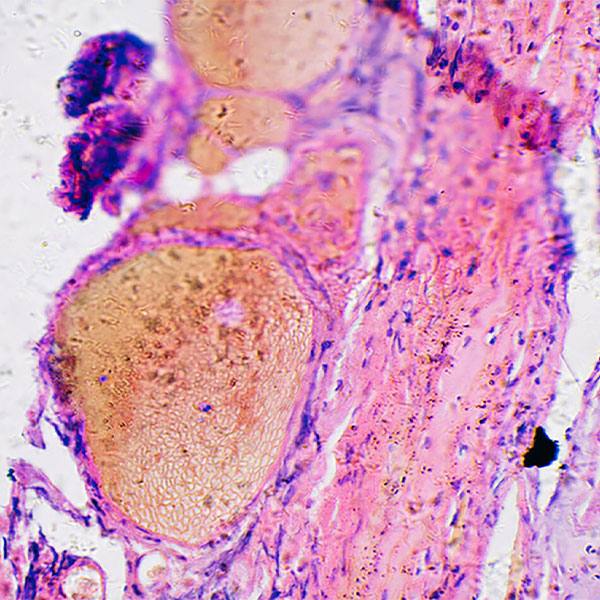
With omics investigations, researchers use a toolkit of scientific precision methods — such as DNA sequencing, microarrays, mass spectrometry and other high-throughput technologies. These technologies can help scientists simultaneously measure and analyze various biological omics molecules at multiple levels deep inside human cells, tissues and organisms — where many diseases evolve.
Envisioning the future of health care visits
As a family physician, Dr. Presutti is already integrating genomics and genetic screening into his everyday medical decision-making for his patients, realizing the potential for detecting inherited genetic diseases, reducing late-stage cancer diagnoses and saving lives.
"If I can help identify those patients at high risk, then we can start screening them earlier and avoid the situation of metastatic cancer and early cancer deaths," Dr. Presutti explains. "At the end of the day, it's not about screening every patient for every disease, because we could probably flood ourselves with data that way. What we want to do is understand who's at risk, and then screen appropriately."
A key part of his effort is integrating Mayo Clinic's genomics experts into his patients' care team to provide education and guidance.
"Here at Mayo Clinic, patients know that the genetic information they're receiving is quality," Dr. Presutti says. "And they feel safe with conversations with our genetic counselors and our medical geneticists."
Ultimately, Dr. Presutti envisions a day when he can incorporate multiple omics into his practice, including pharmacogenomics — the study of how genes affect a person's response to drugs. He says this advanced omics approach could help make patient visits more focused on proactive and preventative care rather than reactive.
Moving omics clinical trials from clinic to people’s homes
Mayo Clinic staff are working hard to increase access to omics-related studies and clinical trials for more people, including underrepresented racial and ethnic minority populations and those living in rural communities. To broaden the reach, clinical trial study staff are already transitioning some omics-related studies out of hospitals, labs, and clinics to take them directly to people in their homes and communities.
This new era of direct-to-patient omics clinical trials is built on a foundation of collaborations with local communities, including local health systems and nontraditional sites, like churches or retail centers.
Thanks to advances in medical tools and technologies, some of the at-home clinical trial processes may include administering experimental therapies, collecting biospecimen samples, conducting mobile imaging, completing electronic survey questionnaires, participating in telehealth video visits and using special medical monitoring devices.
Direct-to-patient clinical trials in the spotlight at 12th annual Individualizing Medicine Conference
The 12th annual Mayo Clinic Individualizing Medicine Conference, called "Direct-to-Patient Omics-Based Clinical Trials" on May 5-6, 2023, in Ponte Vedra, Florida, will bring together some of the world's top scientists, clinicians and thought leaders to share the latest omics and data-driven analytical technologies and research.
"The landscape of medicine is changing," says Konstantinos Lazaridis, M.D., the Carlson and Nelson Endowed Executive Director for Mayo Clinic's Center for Individualized Medicine. "What we thought clinical studies and trials were five years ago is no longer the case. Direct-to-patient omics-based clinical studies are increasing access, leveraging minority engagement, decreasing costs, and ultimately improving patient care. Omics education for providers will update those at the front lines of health care on the most state-of-the-art knowledge in the field."
Learn more
Read more stories about advances in individualized medicine.
Register to get weekly updates from the Mayo Clinic Center for Individualized Medicine blog.
Join the conversation
For more information, visit Mayo Clinic Center for Individualized Medicine, or Twitter at @MayoClinicCIM.

Related Articles