-
Individualized Medicine
Mayo researchers studying ‘promising’ new approach to treating advanced cancer, 1 patient at a time, 1 tumor at a time

A collaborative team of Mayo Clinic scientists is studying an innovative strategy for treating advanced cancer, using genomics and human tumor samples as their guide. The novel approach, called Ex Vivo, creates a miniature cancer replica for testing therapies outside a patient’s body, combined with a comprehensive genomic analysis of a patient’s cancer cells.
“We are now at the cusp of understanding cancer at the individual level, the molecular complexity level, says George Vasmatzis, Ph.D., study leader and co-director of Mayo Clinic’s Biomarker Discovery Program within the Center for Individualized Medicine.
Dr. Vasmatzis says Ex Vivo ultimately tailors the most effective drug, or drug combination, to each individual cancer tumor. He envisions the study leading to a transformation in how patients with cancer are diagnosed and treated.
“We were blind and now we can see,” Dr. Vasmatzis says, “because if you can understand cancer, you can manage it.”
Reshaping precision medicine
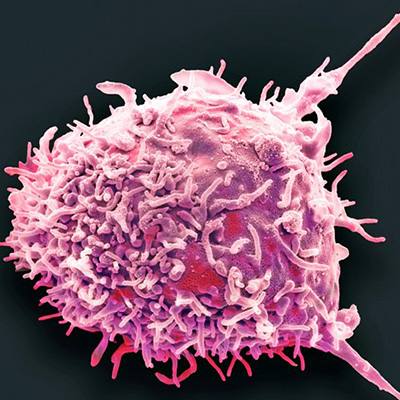
More than 1.8 million people in the U.S. were diagnosed with cancer in 2019, according to the American Cancer Society, and an estimated 610,000 deaths were attributed to the disease. A majority of the cancer deaths were the result of metastases, when clusters of cancer cells circulate and spread to vital organs.

The Ex Vivo strategy centers on finding treatment options where none have existed, by knowing the full story of each tumor and recognizing every patient’s cancer as a unique disease of mutated cells.
A former electrical engineer who has dedicated his career to unlocking the mysteries of cancer, Dr. Vasmatzis says cancer can no longer be viewed as one disease, or even a dozen diseases.
“Because even within the same tumor, different cells can have different genetic changes,” he explains. “Cancer cells evolve and multiply, and when cancer becomes advanced it loses the connection of where it started from — the lung, breast, brain — and it becomes more individual. It is why drugs that are fully effective in some patients provide little or no response in others.”
Ex Vivo in action
The Ex Vivo process starts with taking a small biopsy of a patient’s cancer tumor and dissecting the genetic details at high resolution to find out where the cancer is going and what it is doing. Dr. Vasmatzis says peeling away the many layers of complex information takes a team of highly specialized medical experts in oncology, pathology, biology, genetics and more.
“Our team is carefully constructed to run like an engine, and this is where it happens,” he says, walking through the laboratory, where clinicians and scientists are peering into microscopes, running high-tech machines and studying whole genome images on large computer screens.
"We are now at the cusp of understanding cancer at the individual level, the molecular complexity level." - George Vasmatzis, Ph.D.

“For example, a very sophisticated tissue acquisition team is extremely important in making sure we are extracting the right cell types,” he explains. “We need molecular biology expertise to get billions of bits of data out of the cells and amplify that information for sequencing. Then, you need analytics people and mathematicians to be able to interpret and develop algorithms.”
Dr. Vasmatzis says, many times, the entire lab is focused on just one patient’s cancer.
“One person at a time, one tumor at a time,” he says.
Replicating cancer tumors
After uncovering the cancer’s genomic roadmap, the second part of the study begins with testing existing FDA-approved drugs on the cancer cells.
Overseeing the microcancer portion of the study and co-leading the project is Panos Anastasiadis, Ph.D., a cancer biologist and chair of the Mayo Clinic Department of Cancer Biology, with expertise in cell-to-cell adhesion and cell interactions in cancer tumors.
Dr. Vasmatzis says early results of the first 100 Ex Vivo tests are “promising.”
“Ex Vivo enables us to stay ahead of the cancer instead of behind it,” he says. “This is the way forward for individualized medicine.”
Dr. Anastasiadis and his team use a second piece of a patient’s tumor to create 3-D miniature cancer replicas.

“We separate all the cells that formed that tumor,” he explains. “So whatever that tumor was, now it is individual cells.”
Then, small numbers of cells are divided into liquid droplets, where the cells regroup, he describes.
“The cells that were originally part of the tumor structure were adhering to each other,” he explains. “And they adhere to each other again in the 3-D cultures.”
Dr. Anastasiadis says the cells form miniature versions of the tumor that was originally inside the patient’s body.
“Only now it is outside of the patient’s body and we can test drugs on it,” he says. “And we’re looking for the drugs and drug combinations that target the genomic alterations in each patient’s individual tumor, and that will kill most, or all of the cells,” he explains.
Each miniature cancer model can screen dozens of drug candidates, including combinations not tried before, as well as immunotherapies and viral therapies.
“Using advanced genomics, we usually identify quite a few, maybe 10 to 20 potential targets for treatment,” he says. “Microcancer screening identifies the most effective therapy outside the body. Our theory is that when we treat the patient with this therapy, we will also have a strong response to treatment.”
“Ex Vivo enables us to stay ahead of the cancer instead of behind it. This is the way forward for individualized medicine.” - Panos Anastasiadis, Ph.D.
Strength in numbers
Dr. Anastasiadis emphasizes the strength of Ex Vivo is in doing both parts: the genomics and the miniature cancers. He says doing just one or the other only paints a portion of the picture.
“Through genomics, we know only certain mutations or amplifications, which we call ‘driver genes’ or ‘driver mutations,’” he says. “Knowing just the genomics is inconclusive. You need both.”
He points to the “HER2 protein” in breast cancer as a good example. Patients with human epidermal growth factor receptor 2 (HER2) positive breast cancer, accounting for one in five breast cancer cases, are treated with HER2-targeted therapy, but it is not always effective.
“We don’t know why just 70% of patients respond to the HER2-targeted therapy while 30% do not,” he says. “Complicating things, in most cases you have more than one potential driver, but you don’t know where to target therapy”.
Dr. Anastasiadis says that by testing a drug on the tumor before testing it in the patient can clear these uncertainties. He says Ex Vivo seeks to eliminate the trial and error of patients being exposed to drugs that are often toxic and provide no benefit.
“Ex Vivo is the paradigm we need. There are very few metastatic or advanced cancers for which available therapies provide meaningful longevity." - Minetta Liu, M.D.

From innovation to patient care
After the completion of each Ex Vivo test, researchers and clinicians gather for a comprehensive review, including Minetta Liu, M.D., a Mayo Clinic medical oncologist and research chair for the Department of Oncology.
“Ex Vivo is the paradigm we need,” says Dr. Liu, whose clinical focus is on breast oncology.
Dr. Liu emphasizes the study is not designed to treat patients yet, but when it does translate to clinical care at Mayo Clinic, she believes it could be life-changing.
“There are very few metastatic or advanced cancers for which available therapies provide meaningful longevity,” Dr. Liu says. “Precision drug selection is clearly needed. This will be accomplished through genomics and functional modeling to gauge which therapies will work best for an individual at that particular point in their disease course.”
The Ex Vivo team plans to continue the study for one- to two more years before bringing the procedure to the clinic.
“What I’m hoping is that as we gain knowledge, we will start seeing patterns that will work,” Dr. Vasmatzis says. “We have a lot of work to do to take the next step, but we are all passionate in bringing this to our patients in the near future.”
Stay informed
Want to read more stories like this one?
Register to get weekly updates about new stories on Mayo Clinic Center for Individualized Medicine blog.
Join the conversation
For more information on the Mayo Clinic Center for Individualized Medicine, visit our blog, Facebook, LinkedIn or Twitter at @MayoClinicCIM
Related Articles